The Biopsychosocial Model
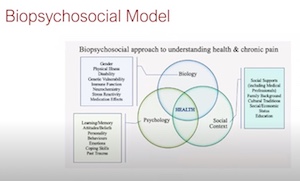
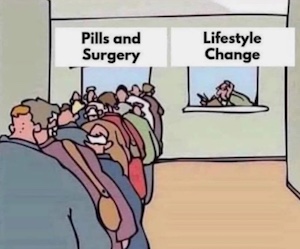
Although very successful in some areas of medical diagnosis and treatment, Western Medicine is based on a bio-medical model which is not well-suited for treating chronic illness or mental conditions related to emotional, social, and nervous system disregulation. By contrast, the biopsychosocial model incorporates cognitive, perceptual, and emotional factors; Central Nervous System modulation; and social interaction when treating patients. Qigong is a biopsychosocial practice and therapy.
Wikipedia: The biopsychosocial model is a broad view that attributes disease outcome to the intricate, variable interaction of biological factors (genetic, biochemical, etc), psychological factors (mood, personality, behavior, etc.), and social factors (cultural, familial, socioeconomic, medical, etc.).

The need for a new medical model: a challenge for biomedicine. The dominant model of disease today is biomedical, and it leaves no room within tis framework for the social, psychological, and behavioral dimensions of illness. Medicine’s crisis stems from the logical inference that since “disease” is defined in terms of somatic parameters, physicians need not be concerned with psychosocial issues which are assumed, mistakenly, to lie outside medicine’s responsibility and authority. A biopsychosocial model is proposed that provides a blueprint for research, a framework for teaching, and a design for action in the real world of health care. Engel. 1977. This is the seminal paper on the biopsychosocial model.
Mind body medicine: a modern bio-psycho-social model forty-five years after Engel. Perhaps the empirical basis of a non-dualistic mind body medicine will advance to the point that ignoring the benefits of a holistic approach will be considered outside the standard of care. The mind body approach includes relaxation response elicitation through meditation, mindful exercise like yoga and tai chi, cognitive skills training, positive psychology, problem solving and acceptance with commitment to eudemonic values and perhaps most importantly social support and pro-social behavior along with spiritual connectedness. These latter 3 aspects flow from secure attachment, the primary foundation for human wellbeing laid down by our mammalian evolution. All these resilience dimensions are enhanced by commitment to a healthy lifestyle that includes avoidance of smoking, excessive alcohol intake and recreational drug use, as well as exercise, sleep hygiene and a low glycemic diet. PMCID: PMC10060142.
The effectiveness of low-dosed outpatient biopsychosocial interventions compared to active physical interventions on pain and disability in adults with nonspecific chronic low back pain (CLBP): a systematic review with meta-analysis. Conclusions: This meta-analysis suggests that low-dosed primary care biopsychosocial interventions has favourable effects in terms of disability and pain intensity compared to active physical treatments alone. All conducted meta-analyses indicate that biopsychosocial interventions produce better outcomes than active physical treatment alone. Therefore, we strongly recommend decision makers and clinical practitioners to analyse how psychosocial elements can be introduced into outpatient (low-dosed) CLBP interventions. PMID: 36565010.

Qigong Mind-Body Exercise (QMBE) as a Biopsychosocial Therapy for Persistent Post-Surgical Pain in Breast Cancer: A Pilot Study. Harvard Medical School research determines QMBE is a safe and gentle multimodal intervention that shows promise in conferring a broad range of psychosocial and physical benefits for breast cancer survivors. Note that they clearly state that Qigong provides psychosocial and not just physical benefits.

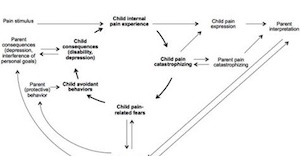
The Pain and Movement Reasoning Model: Introduction to a simple tool for integrated pain assessment. The Pain and Movement Reasoning Model presented in this paper attempts to capture the complexity of the human pain experience. The Model is strongly underpinned by Neuromatrix Theory and incorporates current concepts of neuroplastic determinants on the quality and nature of pain. Consequently, the Model avoids the risk of simplifying elements of the pain experience into linear independent systems e.g. central sensitisation, neuropathic, nociceptive. In a similar way the Model does not separate the biopsycho-social framework into its component parts, but instead integrates the combined influence of the physiological, cognitive, emotional and social inputs on neurophysiological mechanisms. Through consideration of this range of information, the predominant and changeable influences can be identified, leading therapists to select the most appropriate techniques. PubMed.

Pain and the neuromatrix in the brain. Pain is produced by the output of a widely distributed neural network in the brain rather than directly by sensory input evoked by injury, inflammation, or other pathology. The neuromatrix, which is genetically determined and modified by sensory experience, is the primary mechanism that generates the neural pattern that produces pain. Its output pattern is determined by multiple influences, of which the somatic sensory input is only a part, that converge on the neuromatrix.
 The biopsychosocial model of illness: a model whose time has come. The biopsychosocial model outlined in Engel's classic Science paper four decades ago emerged from dissatisfaction with the biomedical model of illness, which remains the dominant healthcare model. Engel's call to arms for a biopsychosocial model has been taken up in several healthcare fields, but it has not been accepted in the more economically dominant and politically powerful acute medical and surgical domains. It is widely used in research into complex healthcare interventions, it is the basis of the World Health Organisation's International Classification of Functioning (WHO ICF), it is used clinically, and it is used to structure clinical guidelines. Critically, it is now generally accepted that illness and health are the result of an interaction between biological, psychological, and social factors. Despite the evidence supporting its validity and utility, the biopsychosocial model has had little influence on the larger scale organization and funding of healthcare provision. With chronic diseases now accounting for most morbidity and many deaths in Western countries, healthcare systems designed around acute biomedical care models are struggling to improve patient-reported outcomes and reduce healthcare costs. Consequently, there is now a greater need to apply the biopsychological model to healthcare management. The increasing proportion of healthcare resource devoted to chronic disorders and the accompanying need to improve patient outcomes requires action; better understanding and employment of the biopsychosocial model by those charged with healthcare funding could help improve healthcare outcome while also controlling costs.
The biopsychosocial model of illness: a model whose time has come. The biopsychosocial model outlined in Engel's classic Science paper four decades ago emerged from dissatisfaction with the biomedical model of illness, which remains the dominant healthcare model. Engel's call to arms for a biopsychosocial model has been taken up in several healthcare fields, but it has not been accepted in the more economically dominant and politically powerful acute medical and surgical domains. It is widely used in research into complex healthcare interventions, it is the basis of the World Health Organisation's International Classification of Functioning (WHO ICF), it is used clinically, and it is used to structure clinical guidelines. Critically, it is now generally accepted that illness and health are the result of an interaction between biological, psychological, and social factors. Despite the evidence supporting its validity and utility, the biopsychosocial model has had little influence on the larger scale organization and funding of healthcare provision. With chronic diseases now accounting for most morbidity and many deaths in Western countries, healthcare systems designed around acute biomedical care models are struggling to improve patient-reported outcomes and reduce healthcare costs. Consequently, there is now a greater need to apply the biopsychological model to healthcare management. The increasing proportion of healthcare resource devoted to chronic disorders and the accompanying need to improve patient outcomes requires action; better understanding and employment of the biopsychosocial model by those charged with healthcare funding could help improve healthcare outcome while also controlling costs.

Is it possible to bridge the Biopsychosocial and Biomedical models? The author writes: Biological, psychological and social factors are in reality integrated and that biopsychosocial medicine seeks to elucidate this reality. The biomedical, organ-based perspective focuses on disease mechanisms and assumes that the psychological and social are not essential to understanding and treating patients, although humanism in patient care is of course endorsed. Bridging these perspectives is important because the biomedical is the predominant model adopted by those who decide how to allocate health care dollars in the United States and many other countries. This in turn determines what clinical care is provided at the bedside.

Mind-Body Medicine: State of the Science, Implications for Practice. Although emerging evidence during the past several decades suggests that psychosocial factors can directly influence both physiologic function and health outcomes, medicine has failed to move beyond the biomedical model, in part because of lack of exposure to the evidence base supporting the biopsychosocial model... there is considerable evidence of efficacy for several mind-body therapies in the treatment of coronary artery disease (e.g, cardiac rehabilitation), headaches, insomnia, incontinence, chronic low back pain, disease and treatment-related symptoms of cancer, and improving postsurgical outcomes. We found moderate evidence of efficacy for mind-body therapies in the areas of hypertension and arthritis.
 Duke researchers declare that interest in the use of psychosocial interventions to help older adults manage pain is growing.
Duke researchers declare that interest in the use of psychosocial interventions to help older adults manage pain is growing.

Non-pharmacological interventions and neuroplasticity in early stage Alzheimer's disease. Non-pharmacological interventions have the potential to reduce cognitive decline and to improve psychosocial aspects in mild cognitive impairment and Alzheimer's dementia, and the absence of side effects makes them a favorable option also for preventive strategies.

Religiosity and Health: A Holistic Biopsychosocial Perspective. The influence of religion and spirituality on health is examined within the context of the holistic paradigm and historical connection between nursing and spirituality. While nursing and spirituality often intersect with end-of-life considerations, this article presents findings from studies that demonstrate that religious involvement favors health and longevity across the life course. Examples include protective associations with stress, depression, self-rated health, and infant birth weight.


 Trends in Yoga, Tai Chi, and Qigong Use Among US Adults, 2002-2017
Trends in Yoga, Tai Chi, and Qigong Use Among US Adults, 2002-2017 "Although not proven conclusively from a Western Medical stand point, Qigong is an accepted treatment option in the fields of complementary and alternative medicine. Qigong treatment is also used extensively in China as part of Traditional Chinese Medicine and has been included in the curriculum of Chinese universities. Qigong practice serves both a preventive and curative function. It is considered to be effective in improving the effects of many chronic conditions such as hypertension, diabetes, allergy, asthma, arthritis, degenerative disk disease, cancer, depression, anxiety and addiction. Qigong works by improving the practitioners’ immunity response, increasing a person’s self-healing and self-recovery capabilities and enhancing one’s self-regeneration potential...." More from Lee Holden:
"Although not proven conclusively from a Western Medical stand point, Qigong is an accepted treatment option in the fields of complementary and alternative medicine. Qigong treatment is also used extensively in China as part of Traditional Chinese Medicine and has been included in the curriculum of Chinese universities. Qigong practice serves both a preventive and curative function. It is considered to be effective in improving the effects of many chronic conditions such as hypertension, diabetes, allergy, asthma, arthritis, degenerative disk disease, cancer, depression, anxiety and addiction. Qigong works by improving the practitioners’ immunity response, increasing a person’s self-healing and self-recovery capabilities and enhancing one’s self-regeneration potential...." More from Lee Holden: 










 The Integrative Veterinary Medicine
The Integrative Veterinary Medicine